Endometriosis affects around 10% of women and girls worldwide during their reproductive years, around 50% of infertile women are impacted by this condition. Among those suffering from pelvic pain, 50-80% may have endometriosis. Despite its prevalence, many women experience significant delays in diagnosis, sometimes waiting 4-11 years for confirmation. This is because endometriosis symptoms often mimic other conditions, making it challenging to identify.
Early diagnosis is crucial to improving quality of life and preventing complications. In this guide, we’ll explore the symptoms, causes, risk factors, diagnosis, and treatment options for endometriosis, aiming to empower individuals with knowledge and support.
Table of Contents
What is Endometriosis?
Endometriosis occurs when tissue similar to the uterine lining (endometrium) grows outside the uterus. While it primarily affects the pelvic region, it can also spread to other organs, including the bladder, intestines, and even, in rare cases, the lungs. This tissue acts like regular endometrial tissue, thickening, breaking down, and bleeding with each menstrual cycle. However, unlike normal endometrial tissue, it has no way to exit the body, leading to inflammation, pain, and scar tissue formation.
This condition can begin with the onset of menstruation and persist throughout a woman’s reproductive years. While some women experience severe symptoms, others may have “silent endometriosis” with no obvious signs, complicating the diagnostic process.
Risk Factors

Several factors can increase the likelihood of developing this condition :
- Older Age: The risk tends to increase as women age.
- Alcohol Consumption: Regular alcohol intake may be linked to a higher risk.
- Early Menarche: Starting menstruation at a younger age can elevate risk.
- Family History: Having a mother, sister, or daughter with this condition raises the risk.
- Infertility: Women struggling with infertility are more likely to be diagnosed with endometriosis.
- Sex During Menstruation: This practice has been associated with increased risk.
- Low Body Weight: Being underweight can affect hormonal balance, contributing to the condition.
- Prolonged Menstrual Flow: Menstrual periods lasting more than seven days can be a risk factor.
- Short Menstrual Cycles: Having shorter cycles may also increase the risk.
What Causes Endometriosis?

The exact cause of endometriosis is still under investigation, but several theories provide insight:
- Genetic Factors: A hereditary link is evident, as women with close relatives affected by this condition are more likely to develop the condition.
- Immune System Dysfunction: A weakened immune system may fail to identify and destroy endometrial-like tissue growing outside the uterus.
- Menstrual Backflow: Menstrual blood flowing backward through the fallopian tubes into the pelvic cavity can transport endometrial cells, leading to tissue growth in abnormal areas.
- Hormonal Imbalances: Estrogen dominance can stimulate the transformation of embryonic cells into endometrial-like tissue outside the uterus.
- Surgical Scars: Endometrial cells can attach to scar tissue from surgeries like C-sections or hysterectomies, leading to endometriosis.
- Nutritional Deficiencies: Deficiencies in magnesium, iron, vitamin B, zinc, selenium, and folic acid may contribute to the condition.
- Environmental Factors: Exposure to chemicals like dioxins and PCBs, which disrupt hormones, may increase the risk of developing this condition.
- Cell Transformation: Other cells in the body may transform into endometrial-like cells.
- Cell Transport: Endometrial cells may spread to other parts of the body through blood or lymphatic vessels.
Common Sites for Endometriosis

This condition primarily occurs in the pelvic region, affecting various structures. The most common sites include:
- Fallopian Tubes
- Ligaments Around the Uterus
- Pelvic Cavity Lining
- Ovaries (one or both)
- Outer Surface of the Uterus
- Area Between the Uterus and Rectum or Bladder
In rarer cases, endometriosis can also develop in:
- Bladder
- Cervix
- Gastrointestinal Tract (lower and upper)
- Rectum
- Vagina or Vulva
Even more infrequently, endometrial tissue may be found in distant organs or parts of the body.
What Are The Symptoms of Endometriosis?
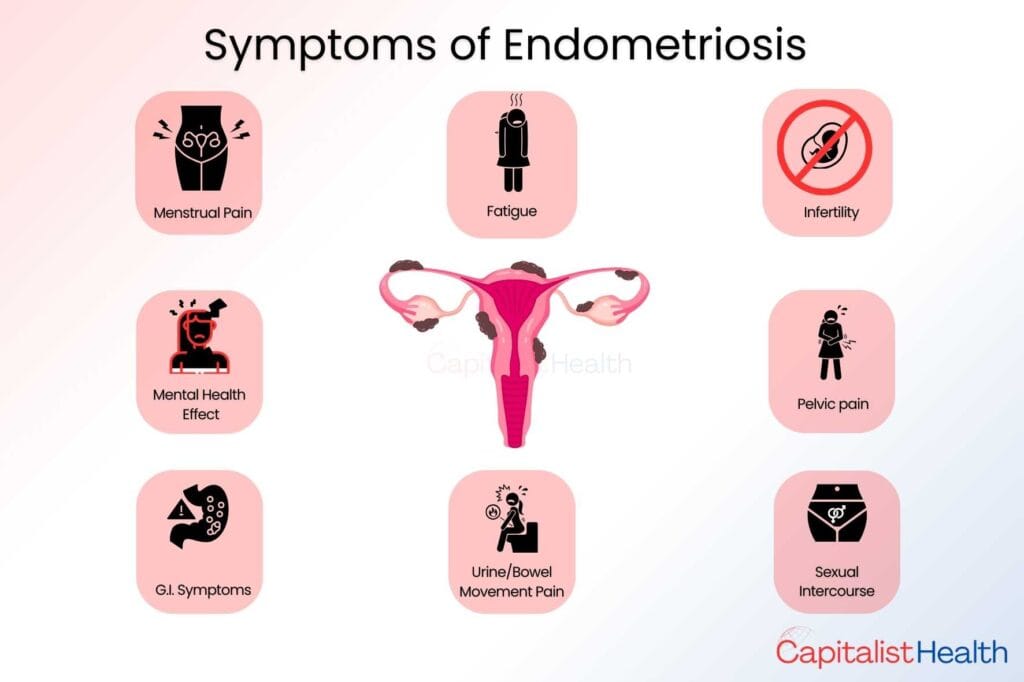
Endometriosis manifests differently among individuals, however, it is primarily associated with pelvic pain, which can vary in intensity, but common symptoms include:
- Severe Menstrual Pain: Often described as debilitating, this pain can worsen over time.
- Pain During Activities: Pain may occur during urination, bowel movements, or sexual intercourse.
- Chronic Pelvic Pain: Persistent pain in the pelvic region.
- Heavy or Irregular Menstrual Bleeding: Including spotting between periods.
- Infertility: Difficulty in conceiving
- Gastrointestinal Symptoms: Bloating, constipation, nausea, or diarrhea.
- Fatigue: Chronic exhaustion that can impact daily life.
- Mental Health Challenges: Anxiety, depression, and stress related to chronic pain.
It’s important to note that symptoms can improve after menopause for some individuals, while others may continue to experience them. Interestingly, up to 30% of individuals with endometriosis may not exhibit any symptoms, known as silent endometriosis, making diagnosis challenging for healthcare professionals.
How is Endometriosis Diagnosed?
Diagnosing endometriosis can be challenging due to its complex presentation and ability to mimic other conditions. The diagnostic process typically involves several steps:
1. Medical History Review: Discussing symptoms, family history, and menstrual patterns.
2. Physical Examination: A pelvic exam to check for abnormalities
3. Imaging Tests:
- Ultrasound (USG): Useful for identifying ovarian cysts.
- MRI Scans: Provide detailed images of the pelvic organs.
- Transvaginal Sonography: Offers a closer look at reproductive organs.
4. Surgical Evaluation:
- Laparoscopy: A minimally invasive procedure to visualize areas affected with endometriosis.
- Biopsy: Taking a tissue sample for pathological examination.
These steps help healthcare professionals accurately diagnose this specific condition and differentiate it from other similar conditions.
A Breakthrough in Endometriosis Diagnosis: What Is PromarkerEndo?
At the 15th World Congress on Endometriosis in Edinburgh, Proteomics International introduced PromarkerEndo, a revolutionary blood test for diagnosing this condition. This non-invasive test boasts a 90% accuracy rate and can detect specific protein biomarkers in patients, even in those without symptoms.
PromarkerEndo outperforms traditional invasive methods by enabling early detection and reducing the chances of late diagnoses. This advancement has the potential to significantly enhance the quality of life for women suffering from this condition, making it a major step forward in managing this chronic condition.
How is Endometriosis Treated And Managed?
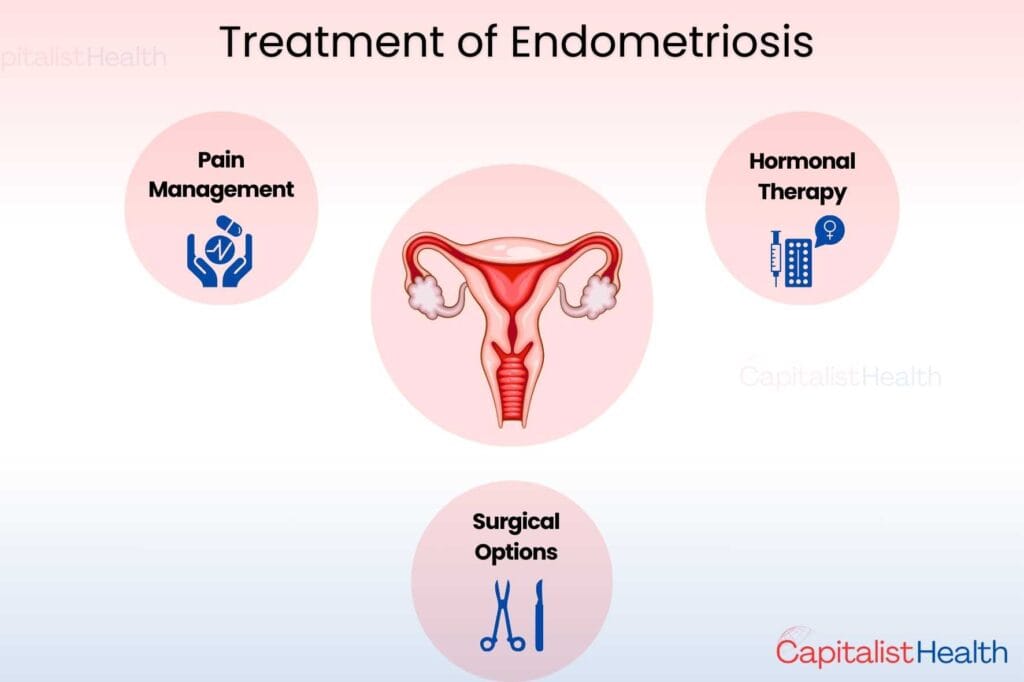
The treatment and management of this condition vary widely based on the individual’s symptoms and the severity of the condition.
1. Pain Management: The primary approach often involves pain relief using non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen. These medications help alleviate discomfort associated with the condition.
2. Hormonal Therapy: For more severe cases, hormonal treatments are commonly used to suppress the growth of endometrial tissue and ovulation. Options include:
- Oral contraceptives
- Progesterone-only pills
- GnRH-analogues
3. Surgical Options: Surgical interventions may be necessary in cases where symptoms are severe or do not respond to medication. This can include laparoscopy to remove endometrial tissue or, in some instances, the removal of affected organs.
4. Individualized Treatment: Treatment plans are highly personalized, taking into account the extent of the condition and whether the individual is considering pregnancy. Those planning to conceive may require different management strategies.
Individuals need to consult with a healthcare professional or specialist to determine the most appropriate treatment options tailored to their specific needs.
How to Lower the Risk of Endometriosis
Research indicates several factors that may reduce the risk of developing this condition:
- Pregnancy: Lower risk in women who have been pregnant.
- Delayed Menarche: Later onset of menstruation.
- Breastfeeding: Prolonged breastfeeding may help.
- Healthy Diet: A diet rich in fruits, especially citrus fruits.
- Hormonal Birth Control: Can lower risk; consult a doctor for guidance.
- Regular Exercise: Engaging in physical activity is beneficial.
- Limit Alcohol and Caffeine: Reducing intake may help.
Conclusion

This condition can deeply affect physical health, emotional well-being, and relationships. Unfortunately, it’s often misunderstood, and many women are encouraged to “tough it out.” But persistent pain is not normal. Seeking timely medical advice is essential for effective management.
By raising awareness, promoting early diagnosis, and supporting each other, we can break the silence and inspire meaningful change.
If you found this information helpful, share it to raise awareness and support others facing endometriosis. Also, were you aware that for much of the 20th century, women were largely excluded from clinical research, click here, To Know more about the Historical Exclusion of Women in Clinical Trials.





2 Comments
Informative blog.
Thanks for your feedback! We’re glad you found it informative.